Day 2: WCRI 35th Annual Issues & Research Conference | Phoenix, AZ
On the second day of the 2019 WCRI Annual Conference, the first session discussed findings and trends of several WCRI studies. State of the States: Selective Findings session included the following speakers:
Moderator: Ramona Tanabe, WCRI: Facility Metrics
Speakers:Carol Telles, WCRIEvelina Radeva, WCRIRebecca Yang, WCRI

WCRI Day 2 Session 1 Panel of Speakers | Photo by Y. Guibert
Facility payments are seen in 26-44% of total claims and represent 9-25% of medical payments across 18 states studies. The median was 17%. There was a wide variation in % of medical payments for facility services by billed place of service. (see Facility slide 1)
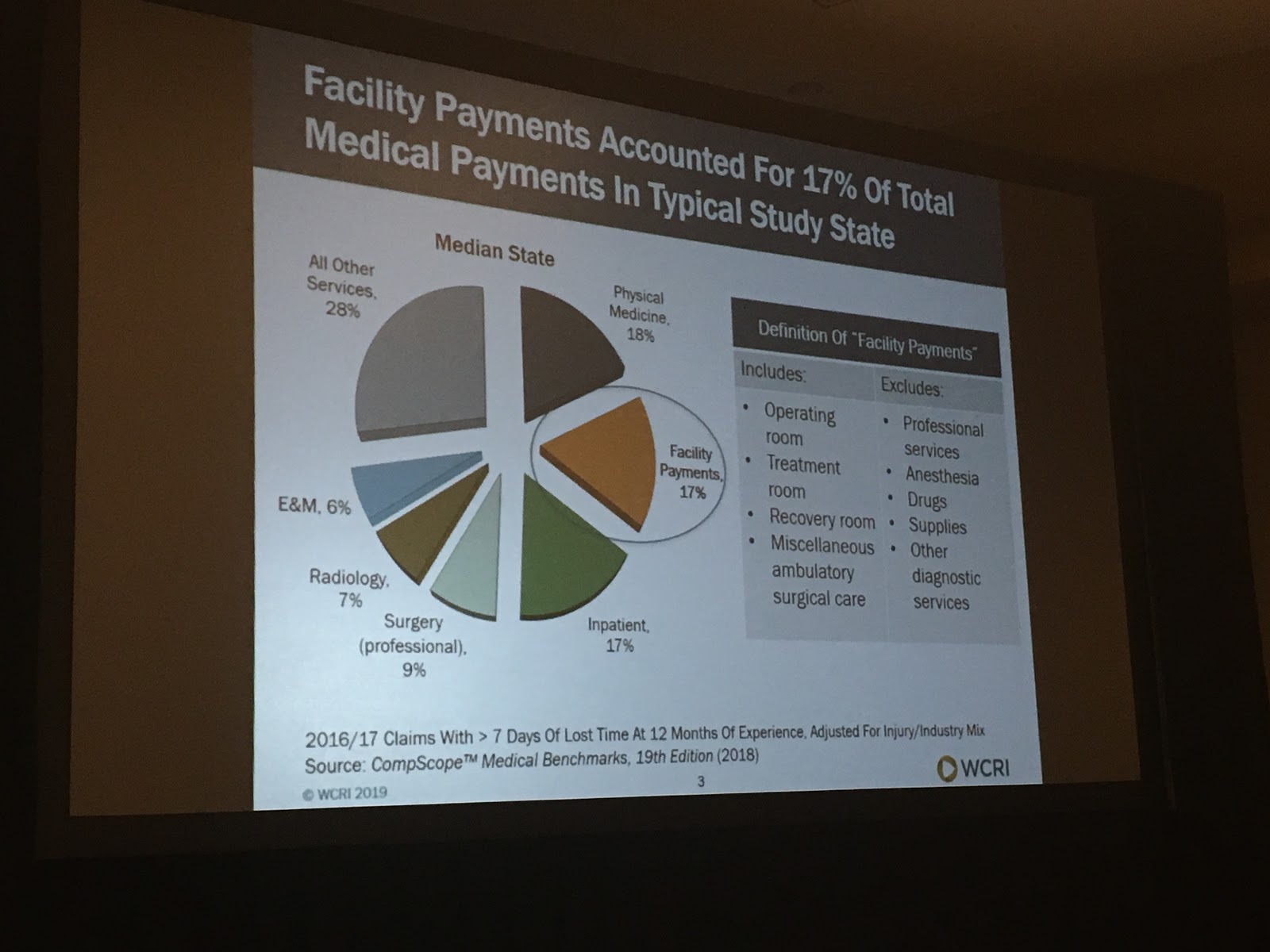
Facility Slide 1 | Photo by Y. Guibert
Ambulatory surgery center (ASC) fees ranged from 4% in MA to 25% in NJ; hospital outpatient fees ranged from 10% in CA to 31% in WI; the average facility payment per claim in the highest states is 4-5x that of lowest states. This was attributed to different reimbursement rules for facilities across the states studied. (see Facility slide 2)
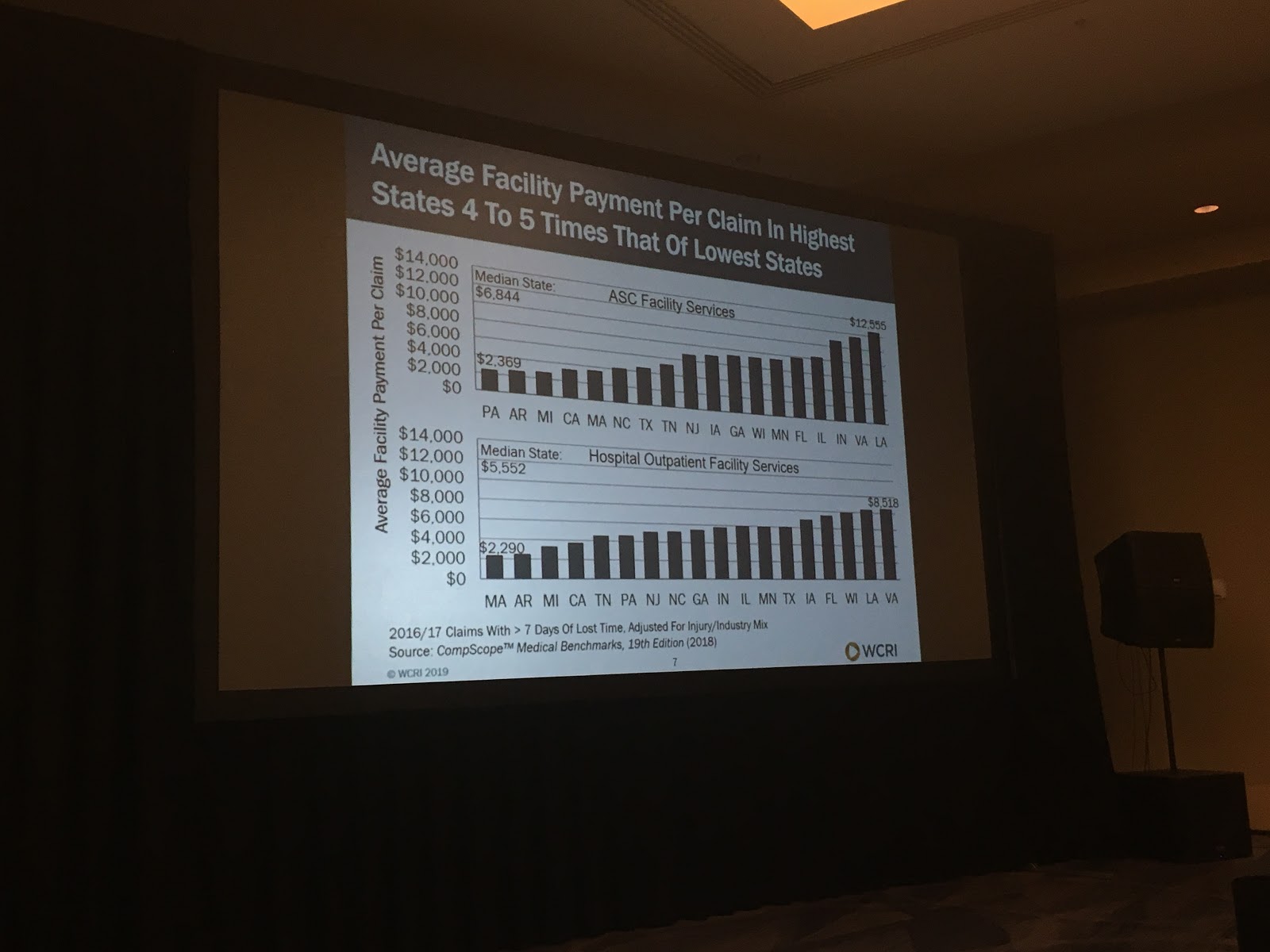
Facility Slide 2 | Photo by Y. Guibert
There was a decrease in inpatient care and a shift from hospital outpatient to ASC facilities during the period 2011 – 2016. It was noted that NC legislation changed their reimbursement fee structure during the study period. The new fee structure went into effect in 2015.
Facility payments make up a sizable share of medical payments in many states 30-35% of claims with major surgery in most states at 12 months; 35-40% at 36 months.
The study found there was a slight decrease in major surgeries: includes invasive surgery ranging from 2-5% in many states 2011-2016.
Possible reasons for the decrease in surgery rates:
- Alternatives to surgery
- State-specific initiatives and active payor management
- Change in the injury mix
The percent of low back disc cases with surgery decreased in most of the study states.
Evelina Radeva, WCRI: Benefit Delivery Expenses
Study on Benefit Delivery Expenses (BDE)
Average claim for minimum 7 days lost time = $42,000. In addition to
medical and indemnity expenses, BDE cost make up a significant portion of the claims in workers’ comp. In a typical state, indemnity costs made up 44% of total costs, medical was 41% and BDE was 15%. (see BDE Slide 1) About half the BDE costs were made up of litigation, the other half were made up of medical management fees, e.g. bill review, UR and nurse case management.
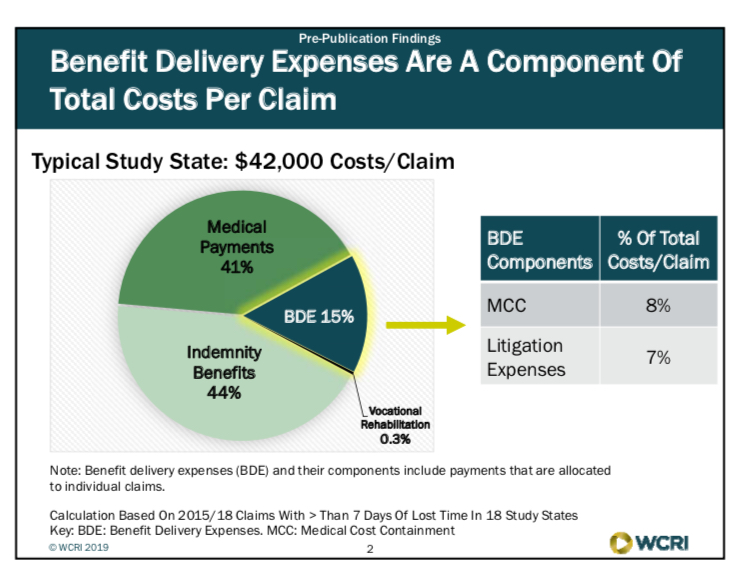
BDE Slide 1
BDE expenses are made up of mostly two types of services:
Medical cost containment
- Bill review
- Utilization review
- Case management
- Provider networks
Litigation Expenses
- Defense attorney payments
- Medical-legal expenses (IMEs, medical testimony, depositions)
- Other (copying, transcription fees, interpreters)
Across the states included in the study BDE accounted for 11% (WI) – 23% (CA) of total costs per claim in 2015 / 2018. In dollars, fees ranged from $4208 on the low end (WI) and the high end, nearly $12,000 per claim (LA).
In most states, medical cost containment was 15-20% of medical-related payments per claim
Ranging from $12k in MA to $31k in LA (see BDE Slide 2).
It was noted that the variance in fees was likely due to the different
medical cost containment strategies employed among the study states:
- Medical fee schedules
- Pharma fee schedule
- Treatment limits
- Utilization review
- Treatment guidelines
- Managed care
- Choice initial provider
Defense attorney payments were the largest share of litigation expenses in most states with fees ranging from $2.8k in TX to $9.5k in LA (See BDE slide 3). Texas system includes ombudsmen to assist injured workers amongst other resources which has resulted in greatly reduced litigation fees.
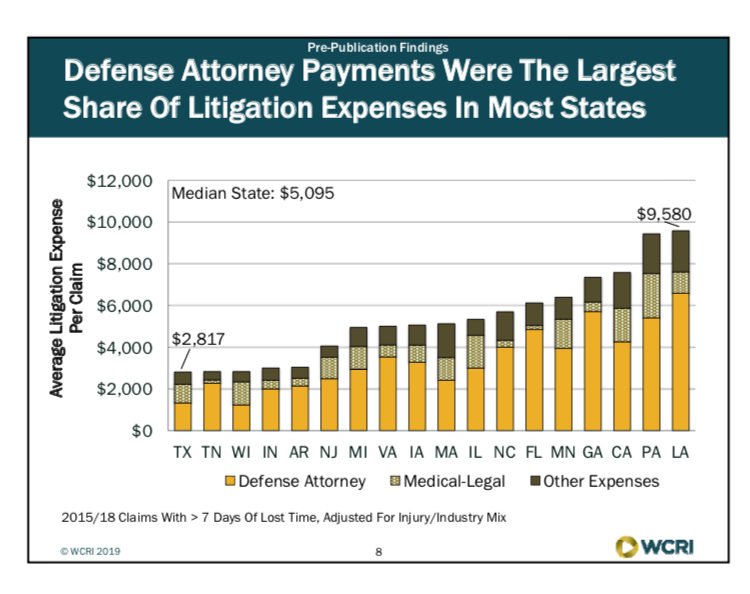
BDE Slide 3
System features driving differences in litigation expenses per claim among states
- Are participants able to easily navigate the system?
- Informal vs. formal dispute resolution process
- Design of the process to determine whether PPD benefits will be awarded, and the level of benefits
- State agency monitoring of dispute resolution and timelines of first temporary total disability payment
BDE per claim grew about 4-6% since 2005 in most study states; NJ and LA had highest increases among the study states; MN had the least increase.
Median Study State: small growth in % of claims with litigation services; payments grew 4-6% / year since 2005
Key Findings
- BDE were 11-23% of total costs per claim among study states in 2015 (evaluated 2018)
- Average BDE per claim affected by medical cost containment strategies, system features and dispute resolution process
- BDE per claim grew about 4-6% per year in most study states 2005-2015 (at 36 months)
Rebecca Yang, WCRI: Frequency and Cost of Lump-Sum Settlements
Rebecca presented findings on WCRI’s study of frequency and costs of lump-sum settlements. Of the states reviewed there were generally two types of indemnity benefit systems: Wage-Loss vs. PPD and 2 states that represented a hybrid of both. (See Lump Sum Slide 1)
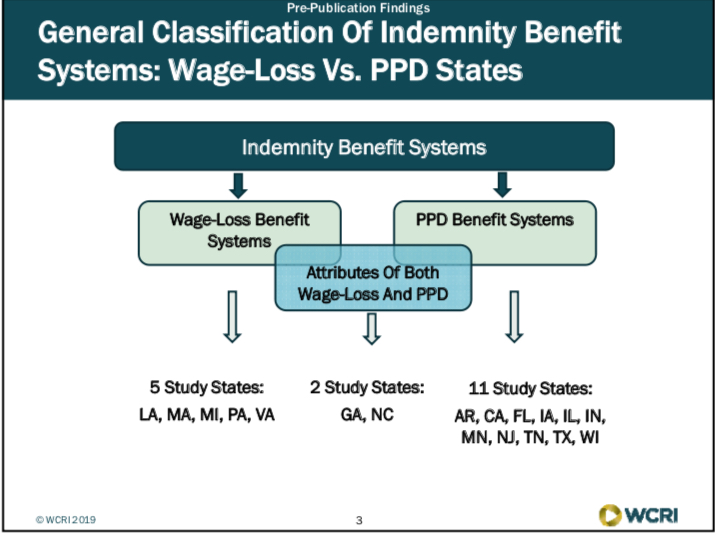
Lump Sum Slide 1
Wage Loss Benefit Systems: 5 Study states: LA, MA, MI, PA, VAPPD Benefit Systems: 11 study states: AR, CA, FL, IA, IL, IN, MN, NJ,TN, TX, WIAttributes of Both wage loss and PPD: 2 study states: GA, NC
State variation in frequency and amount of lump-sum settlements
reflects the benefit structure and other factors, e.g. states with
wage-loss benefit systems had higher settlement amounts.
Timing of settlements varies across states: were earlier in FL, TX, GA; later in MI and NJ (see Lump Sum Slide 2)
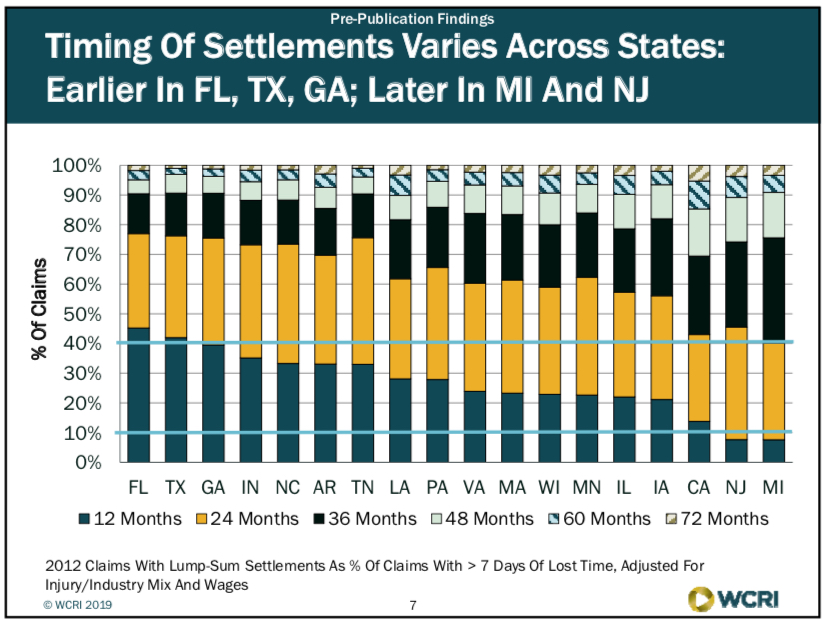
Lump Sum Slide 2
Factors that may influence trends in lump-sum settlement frequency and costs in WC claims:
- Policy changes addressing income benefit payments
- Change in speed of dispute resolution, settlement approval or attorney involvement
- Change in factors that influence workers, payors and attorneys to seek settlements
The percent of claims with lump-sum settlements increased in most
study states since 2008. Settlement amounts per claim remained stable in most states.
CA: longer term increase in lump sum frequency; earlier settlements post SB 863.
FL: faster recent growth in settlement amounts may be related to early effect of court decisions.
WCRI Day 2 | Session 2: Challenges & Opportunities of Telemedicine
Moderator: Dr. David Deitz, David Deitz & Associates
Speakers: Ms. Amy Lee, Texas Dept of InsMr. Kurt Leisure, The Cheesecake FactoryMr. Dan Allen, Construction Industry Service Corp (CISCO)Dr. Stephen Dawkins, Caduceus USA
I appreciated the creative and engaging method WCRI used to draw
the attendees back into the session room from the break. They played a video clip from the movie Casino Royale…the James Bond poisoning scene… he used a remote monitor to restart his heart.
Telemedicine: What we don’t know:
- No quantitative data on use in wc
- Quality trade-offs: most QOC data are “non inferiority”
- Appropriate regulations and reimbursement models?
- Privacy, liability, employee choice, etc.
The Cheesecake Factory launched telemedicine approximately one year ago.
Telemedicine — the process:
- Injury occurs
- If 911 – proceed to Urgent Care / ER
- If non-urgent:
- Nurse triage
- If unsuccessful and non-emergent, escalate to Telemedicine via mobile device
- If telemedicine fails, proceed to UC, ER
Potential Benefits for EE:
- Immediate medical care — no waiting room
- Flexibility of treatment – another option
- 24 hours a day / 7 days a week accessible
- More focused attention from doctor
- No MRSA exposure
- Bilingual doctors available
- Rx to the pharmacy of ee’s choice
- RTW with minimal disruption — may never have to leave the injury location
- Notes from nurse triage to transfer to tele Dr
- Mobile device obtains visual for Dr
Potential Benefits for Employer:
- No transportation issues
- Immediate care for valued ee
- Costs are set per call, less $ than UC/ER
- Injury notes transferred to intake system
- Measurable hard $ results
- No repricing fees
- Keeps ee away from med/legal mills
- Financial savings could be significant
- Medical care is consistent with group ins benefits
- No need to cover shift or pay thru end of shift
Potential Risks:
- Program not successful — too many claims referred to UC/ER from telemed
- Wi-Fi or camera expense / connectivity (not an issue for Cheesecake)
- Privacy concerns — need a private location (office / restroom)
- Adoption by injured staff
YTD Actual Results for Cheesecake (Feb 2018 implementation):
- 3,336 calls into nurse triage
- 1,078 successful triaged by nurse – 32%
- 470 (21%) of remaining 2258 injuries offered telemedicine by nurse triage
- 326 (69%) accepted telemedicine
- 188 (57%) successfully treated through telemedicine and needed no further treatment
- $153K in hard dollar savings in 2018
Opportunities / Lessons Learned / learning:
- Triage needs add’l algorithms to identify telemedicine candidates
- Will take time for staff to trust program
- Internal marketing
- Work with group ins telemed program
- Cultural trust issues
- Ipad concept was “clunky” cont’d automation is critical
- Approval by IWs is high
- More engagement by Dr
- Convenience factor is HUGE
Amy Lee – Texas Dept of InsuranceFrom the regulators perspective; issues that we have had to learn / grapple with…
Senate Bill (SB) 1107:
- Passed in 2017 (not a wc bill)
- Changed the way TX Med board regulated telemedicine services
- Required joint rulemaking between various practitioner licensing boards
- Included requirements for fully insured health plan
Amy reviewed and discussed Texas DWC rulemaking considerations
which include existing WC statutory requirements, billing and reimbursement structure, evidence-based treatment guidelines and pharma formulary (ODG in Texas), UR requirements, health care networks and dispute resolution.
She then discussed Texas DWC rulemaking goals which is to promote statutory system goals including:
- Provide timely, appropriate and high quality medical care to IWs to facilitate RTW
- Timely and cost-effective income and medical benefits
- Taking advantage of technology to provide highest levels of service
- Expand access to telemedicine using current medical billing and reimbursement structure
- Defer to state licensing boards on scope of practice issues
- Preserve IWs statutory choice of treating physician
- Provide clear guidance to healthcare providers and insurance carriers to
- Minimize fee disputes
- Enable data collection and outcomes tracking
- Address medical care — not medical – legal examinations
Telemedicine Utilization in TX:
- Workers’ comp study planned for 2019
- Data since Sept 2018 still preliminary:
- Less than 100 claims
- 31 insurance carriers
- Fewer than 200 medical bills
- Mostly office visits / consultations
- Focus on non-rural areas of the state
She discussed Texas new rule §133.30, effective for services provided on or after September 1, 2018. For more information on this new Texas rule visit the TDI website here.
In closing, Amy discussed future policy considerations:
- Monitor changes to Medicare list of services that can be performed via telemedicine
- Evaluate impact of telemedicine on:
- Medical costs and utilization
- Access to care, especially underserved areas of Texas
- RTW outcomes and IW satisfaction
- Ensure medical data are collected and reported correctly to enabling tracking of costs and outcomes.
I had to scoot out early from this session to catch my flight as Amy was wrapping up her discussion. So the remaining information here is culled from the Twittersphere….
WCRI @WCRI: “Dan Allen from @CiscoBuildUnion says construction
workers don’t have days off…so they may embrace telemedicine if they can get the care they need fast.Younger workers may be open to it, but older workers will probably reject it and opt for a traditional visit.”
Tom Kerr @Tomker11: “Dr. David Deitz said that 1/100th of recent patient visits were done through telemedicine, where as much as 30% could be done through telemedicine. So there is tremendous opportunity for growth.”
Insurance Research @III_Research: “It’s crystal clear […] that telemedicine is a tsunami that will change the practice of medical care.” Dr. Stephen Dawkins gives a provider’s perspective on telemedicine.
Mark Walls @wcmarkwalls: “Takeaways from #WCRI19 telemedicine panel:
- Clear advantages with access to care, especially underserved areas.
- Know your goals. Not necessarily cheaper. But faster and more convenient.
- Regulatory challenges around scope of care and reimbursement.
- Employee adoption key.”
A day and a half of WCRI sessions presented by really smart people and filled with fascinating data, research and observations. This is becoming one of my favorite events of the year. I guess that means I’m becoming a WC nerd. Great to see everyone! See you next year.
Marketing Services
Event Marketing
Conference / Exhibit Services
Brand Management
Media Relations
Digital Marketing
Social Media Management
Google Ads
Custom Programming
SEO Organic Search Strategy
Website Development
WordPress Everything
Web Hosting
Contributors
Want optimum results from your marketing?
Contact us right here
Networking Do’s and Don’ts
Why don’t we educate employees during the ”honeymoon” stage?
Jobs which will grow have many foreign-born workers.
Breaking the Negativity Habit.
Discussing Sensitive Topics with Injured Workers. Part 2
Discussing Sensitive Topics with Injured Workers. Part 1
Crafting the perfect social media post!
10 Tips for a Better Media Interview
The world according to Zachry.
Catching up with Billy Parker, safety advocate…
Texas Legislative Update: Part Deux
Rethinking Pain from the Neck Up
Niche Metrics: Are you reaching the right target audience?
Case Managers: are we “professionals?”
Day 2: WCRI 35th Annual Issues & Research Conference | Phoenix, AZ
Day 1: WCRI 35th Annual Issues & Research Conference | Phoenix, AZ
Debunking MSA Myths…
Prepping for a media interview
Update on the Texas Workers’ Comp System
Injured Worker Advocacy and Why it is Important
Case Management and Value Based Care
SEO: Choosing the Right Internet Marketing Company
My name is Yvonne and I’m addicted to sugar…
Workers’ comp is scary…
Why perception matters…
Have you plugged into Comp Laude® Awards & Gala? There’s still time…
Texas Work Comp: ICT Austin Seminar
Reflections: WCI 2018 and Costa Rica
Opioids: how will new state laws and regs affect my WCMSA?
Keeping your employees at work during rehabilitation…
Case management in WC should be moving toward value-based care
WCMSA Legislation - a Band-Aid Solution?
Workers’ Comp Around the World
Embracing mental health in workers’ compensation…
Next-Gen Workers’ Comp Adjusters: Who will step up?
Next-Gen Workers’ Comp Adjusters: Who will step up to solve this puzzle?
Digital Pills, Return to Function and Boosting Resilience
What happened to resilience training?
Making connections in Wall-e world; and have you heard the goldfish theory?
I’ve still got Texas on my mind…see what Joe Paduda, David Langham, Linda Van Dillen and Ralph Gonzalez are thinking.
Go Big! or Better in Texas? Recap of RIMS Conference in San Antonio.
WC experts talk better media interviews, workforce readiness and shining when you are put on the spot…
Value Based Care, CA considers location-based reimbursement, Sleep and more…
Takeaways from Boston / WCRI 2018: week of 3.19.18
Experts weigh in on Opioids, Opioids, Opioids and CWCI! Week of 3.12.2018
Bias in the Workplace and other expert thoughts 3.9.2018
Is there a place for telemedicine in workers’ comp?
WorkCompRecap Week of 2.12.2018
WorkCompRecap @expertsinwc Week of 2.5.18
WorkCompRecap @expertsinwc Week of 1.29.18
WorkCompRecap: Week of 1.22.18 Twitter @expertsinwc
WorkCompRecap – week of 1/15/18: Twitter @expertsinwc
